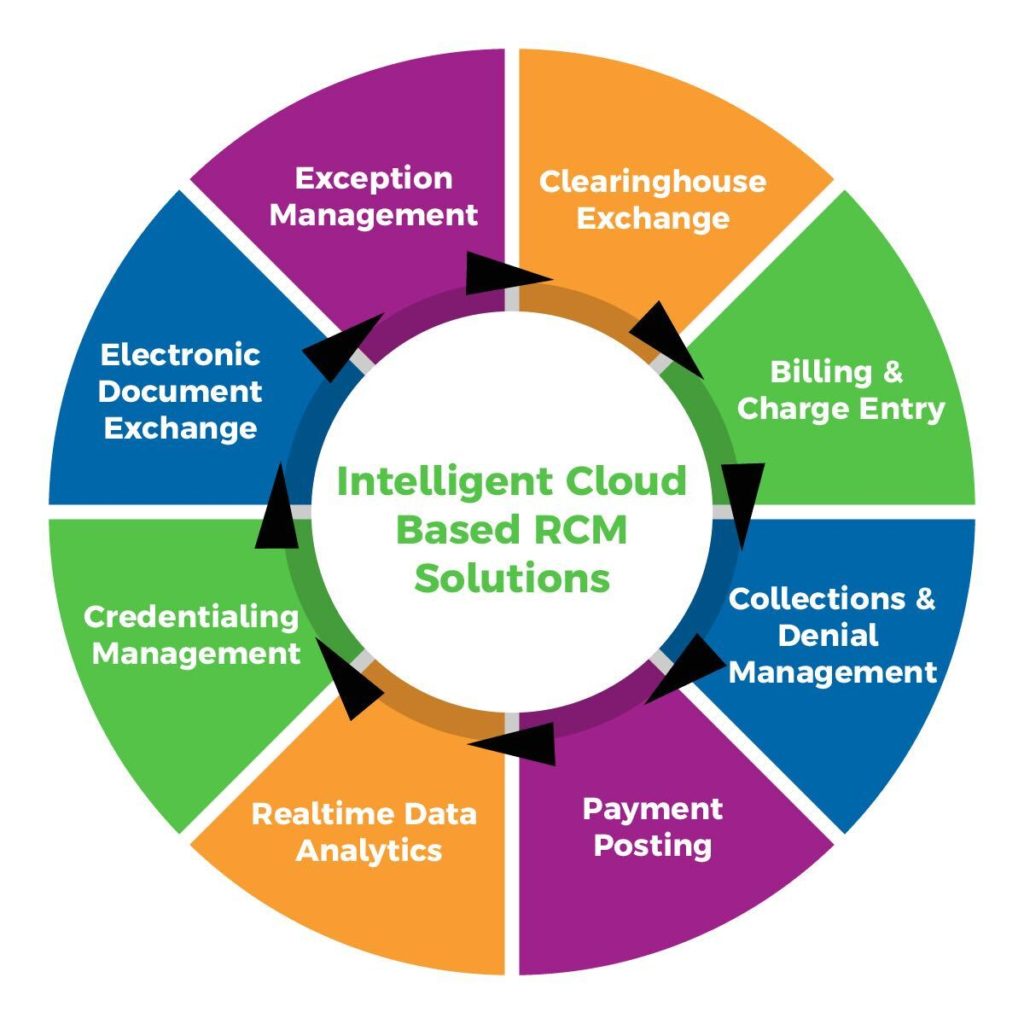
Intelligent Cloud Based Revenue Cycle Management
MDiQ offers complete end to end revenue cycle management services and integrated technology solutions to healthcare organizations. Our solution adapts, optimizes, and scales to small & large provider groups, specialist, laboratory, and ambulatory surgical centers. Our cloud-based system provides the tools and resources you need to optimize your revenue cycle to increase financial and operational performance.
Our Modules, One Automated Workflow
The MDiQ platform is built on the latest internet technologies to create a cloud-based system that is delivered entirely as a modular service. We provide and manage the infrastructure, software, and the hosting of the platform. You simply subscribe to the modules your need, plug in, and see all aspects of your revenue cycle from the device of your choice — be it a desktop PC, tablet, or smartphone. Our cloud-based system provides the tools and resources you need to optimize your revenue cycle to increase financial and operational performance.
Direct <-> Connect Module
Direct <-> Connect is our basic clearinghouse transaction module for managing all types of input and output between all types of health-care organizations. This is our fully integrated clearinghouse solution using real-time, near real-time, batch, fast batch, or any other speed of file synchronization available, featuring connections to all payors in standard and non-standard formats.
Charge Entry & Billing Module
We process all claims in an electronic format, whether received via our Direct<->Connect Module or paper charge sheet from a lock box, scanning process, or other paper source and converted by OCR technology to a digital transaction. Because we treat everything as a digital transaction, all transactions are processed through the business rule engine to automate traditional billing steps such as coding, pricing, payor specific rules, and critical field validation, and then are transformed to a HIPAA-compliant claim format and extracted electronically to carriers for payment. Exceptions are managed (reviewed and trended) so business rules can be modified or developed to eliminate chronically recurring issues. This process allows faster processing, maintains data visibility, and helps minimize human touch points.

Denial Management
MDiQ Denial Manager Module identifies and accounts for all payor denials to target problem areas that affect the bottom line to assure collection of all receivables due from payors. Our Denial Manager Module also allows healthcare organizations to organize and manage remittance inventory; helps staff arrange, prioritize and monitor denials and underpayments; and allows the accurate reporting and viewing of the denied and adjusted amounts. With the information produced by our Denial Manager, healthcare organizations streamline the denial management process by determining root causes, breakdowns in the workflow process, and patterns responsible for denials. All this enables us to establish corrective steps to prevent future revenue loss or delay
Collections
MDiQ Collection Module is a rule-based workflow engine with configurable work queues and the ability to prioritize work based on aging, uncollected claims by client. The module processes claim status messages for the most accurate disposition and pinpoints the bottle neck in the revenue cycle payment process. Unclean claims that are not paid after being processed by the payor are sent to an exception queue to be reviewed, fixed, and re-submitted. Errors are minimized because we use a payor-specific and best practices business rules engine during the billing process. The work queues are configurable by age bands to increase the priority as the claim ages, and notifications and alerts are generated based on client’s requirements or age points. All errors are trended, and business rules are written to automate the collection process to ensure re-occurring errors are remediated for future collections.
Posting & Reconciliation
Electronic transactions received via our Direct<->Connect Module or paper EOBs received via lock box service, scanning process, or other paper source, are converted by OCR technology to a digital transaction. All transactions are digitized and processed through the business rule engine to automate posting payment, adjustments, and reconciliation at the check level, claim level, and service line, balanced to check deposit. Exceptions are reviewed and trended so business rules can be applied to eliminate reoccurring issues, all with minimal human touch points.
Reporting & Analytics
With the proper visibility, payers and healthcare organizations can gain valuable insight into their revenue cycle processes. With MDiQ Healthcare Business Analytics, specialized reports delivered in real-time, helps you make informed decisions about claims and correspondence, identify and remedy exceptions, manage revenue, member, and healthcare organization information, as well as government-required reporting in one interface.

Document Management
For pennies per page, MDIQ lets you treat paper documents just like digital transactions. We convert data, index fields, store documents for viewing, and route paper documents for editing with seamless ease. We can take in paper and give you an all-digital feed, and we can take an all-digital feed to produce the paper documents that you are currently sending. Either way you can keep your environment as digital as you can imagine with clean data, better turnaround times, more reporting and visibility, and truly benefit from a standardized environment.
Credentialing & Contract Management
Our experienced team understands the world of both the payors and healthcare organizations. We help our clients by navigating through the tedious and complex process established by all insurance networks – federal, state, and commercial payors. Whether your practice or provider needs be credentialed for the first time or timely re-credentialed, MDiQ is a reliable resource with an experienced team to gather, validate and confirm each piece of critical data in the credentialing and contracting process We provide credentialing and enrollment management services for healthcare organizations of all types including physicians, nurse practitioners, physician assistants, therapists, laboratories, imaging centers, ASCs, and hospitals. We take care of everything needed to ensure your providers and facilities stay compliant with insurance payors and accrediting organizations. Our credentialing maintenance service is a great fit for organizations seeking help to maintain credentials and their status with the various insurance payors. This includes CAQH credentialing & maintenance, Medicare revalidations and commercial insurance recredentialing.
Exception Management Task List
Exception Management Task List is custom workflow for identifying, segragating, and routing transaction errors to the most cost-effective point of resolution. The overwhelming conventional wisdom has been to maximize the good data and speed it through as fast as possible while letting bad data fall out into a pile to be dealt with manually by highly paid resources. Errors were commonly fixed individually, and on the fly, by inexperience or numerous workers. Group routing, batch-fixing, knowledge management, and upstream rules-based processing weren’t feasible. Our exception management logic tracks and reconciles critical control points, and even our basic set of reports gives you visibility into the exact path every transaction takes. you can derive, change, or reroute data on demand, automatically. Even combined with our Document Management services, you can even treat paper transactions the same as electronic ones.
Electronic Document Exchange
Electronic Document Exchange is a integrated secured portal for uploading documents to the MDiQ Platform. We convert data, index fields, store documents for viewing, and route paper documents for editing with seamless ease. Documents are uploaded by document type and indexed automatically eliminating manual intervention. MDiQ business rules engine based on each client’s unique rules inspects the uploaded document to determine the appropriate workflow process.